Overview / Multidisciplinary Approach
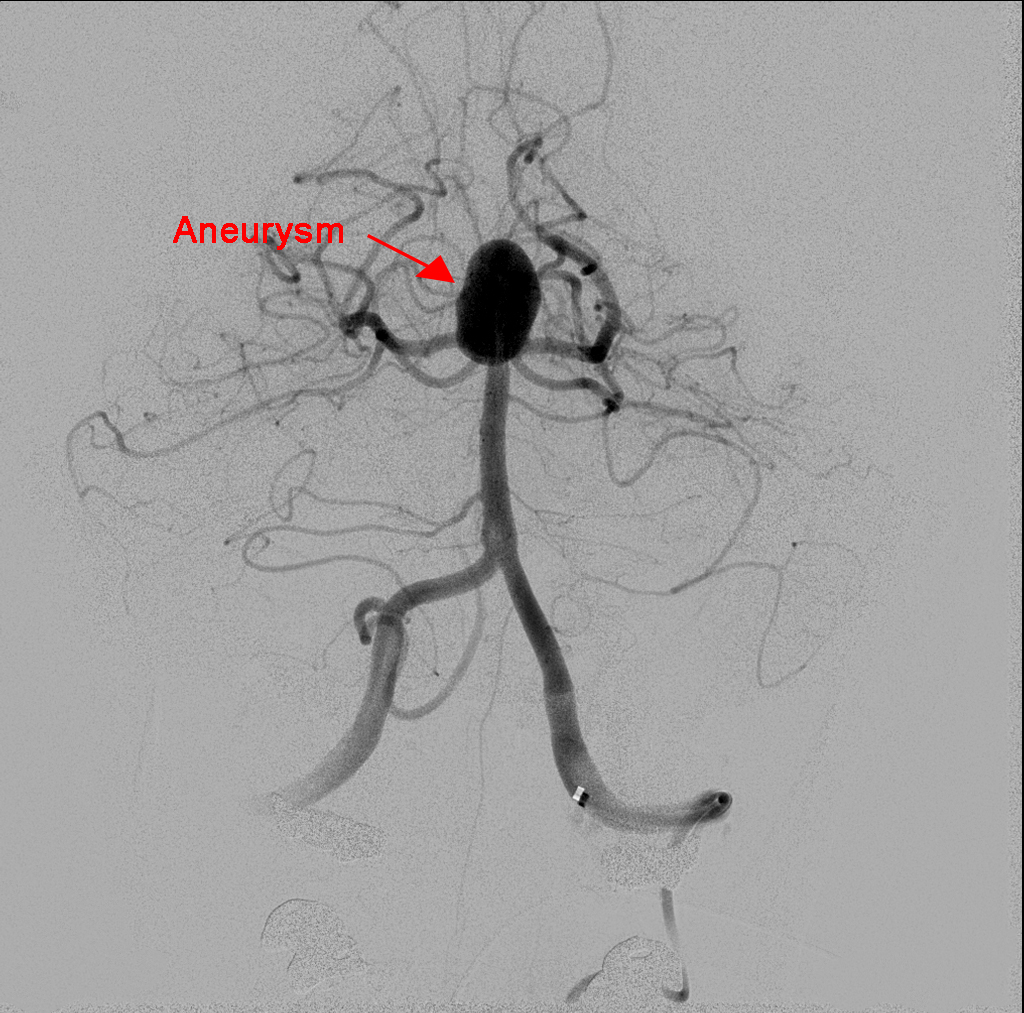
A brain aneurysm is a ballooning or bulging out of an artery where the wall is weak. A brain aneurysm may allow blood to leak into the subarachnoid space around the brain, causing damage to brain cells. If the aneurysm bursts, it can cause an incredibly serious and potentially fatal condition. When aneurysms rupture in the brain, the resulting hemorrhage can cause stroke, coma, brain damage or other life threatening problems. In fact, approximately forty percent of ruptured brain aneurysms are fatal and only twenty percent of patients survive with no permanent damage. There is no clear reason why a brain aneurysm forms, but there are many things that can contribute to its development. Risk factors such as: smoking, hypertension, family history, traumatic head injury and other disorders may increase a person’s risk of developing an aneurysm. It is impossible to predict if and when a rupture of a brain aneurysm may occur.
The risk of suffering a brain aneurysm can be reduced through a series of lifestyle changes that include: not smoking, exercising regularly, eating a balanced, low fat diet, getting help for alcohol and/or drug abuse, and controlling high blood pressure. While aneurysms occur in all age groups, their incidences steadily increase for individuals over age 25, and are most frequently found among those 40 to 60 years old. In addition, women are more likely to have aneurysms than men.
Treatment options for brain aneurysms are determined by the size, shape, and location of the aneurysm in addition to the patient’s age and overall health.
A ruptured brain aneurysm is a life-threatening event requiring emergency medical treatment. A significant symptom is a sudden, severe headache that is often as described as the “worst headache” ever.
Other symptoms may include:
• Stiff neck
• Drowsiness
• Nausea
• Vomiting
• Mental confusion
• Dizziness
• Vision problems
• Traumatic brain injury
Unfortunately, many aneurysms are discovered only after they rupture, because people with unruptured brain aneurysms often have none of these symptoms.
Comprehensive Care Center
Surgical Clipping
Surgical clipping, also called open microsurgery or craniotomy, is an open surgery performed through a surgical opening in the skull. Using an operating microscope and tiny instruments, the surgeon attaches a small metal clip at the base of the aneurysm. Because blood is prevented from flowing into the aneurysm, the chances of it rupturing are greatly reduced. Recovery time is typically four to six weeks.
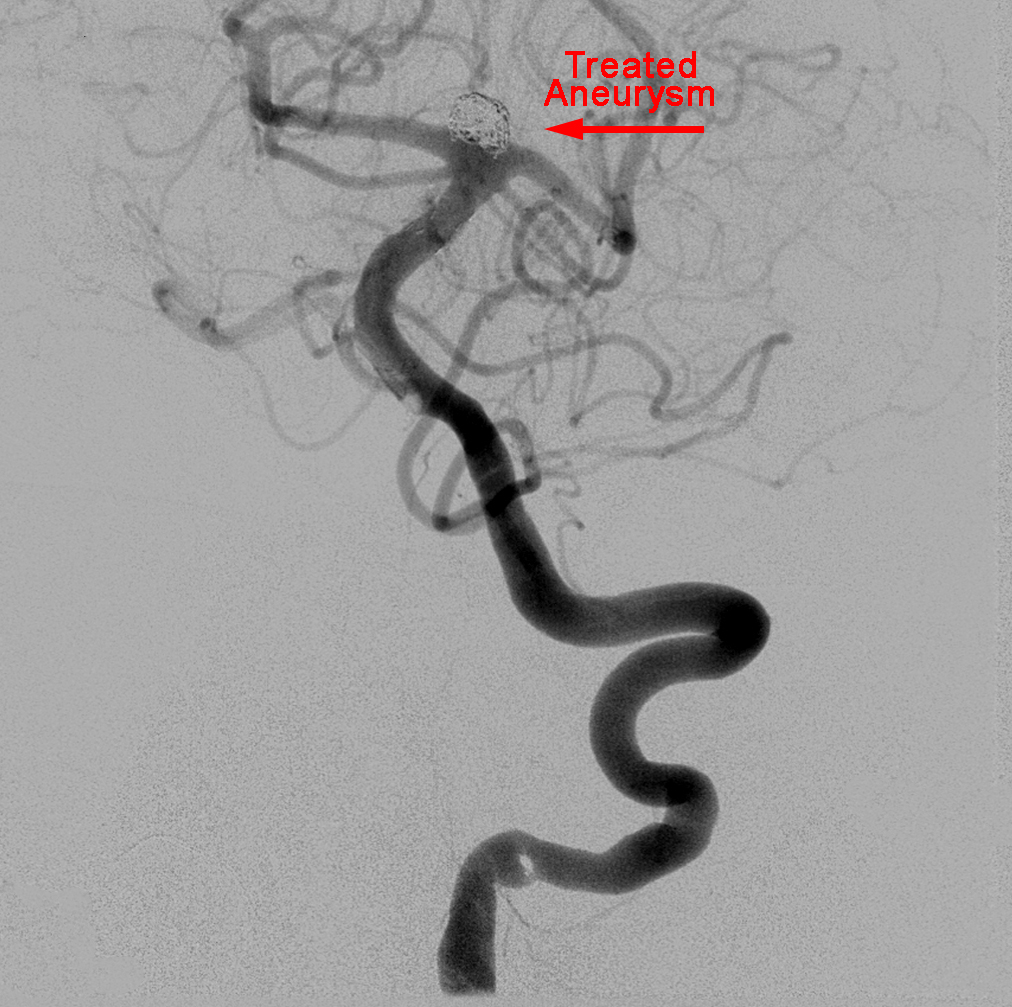
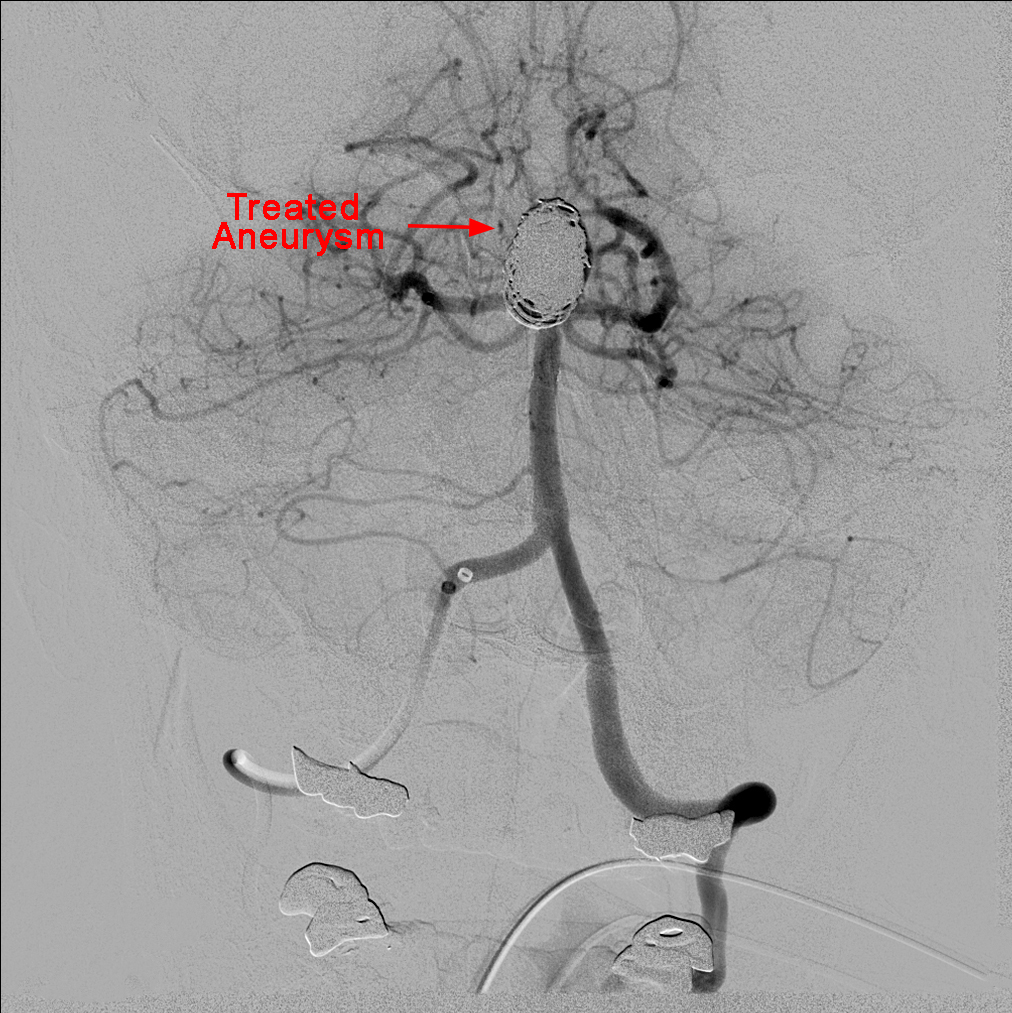
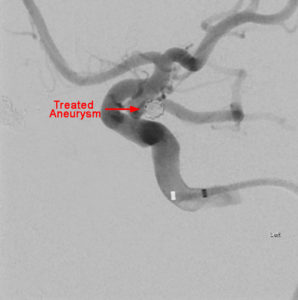
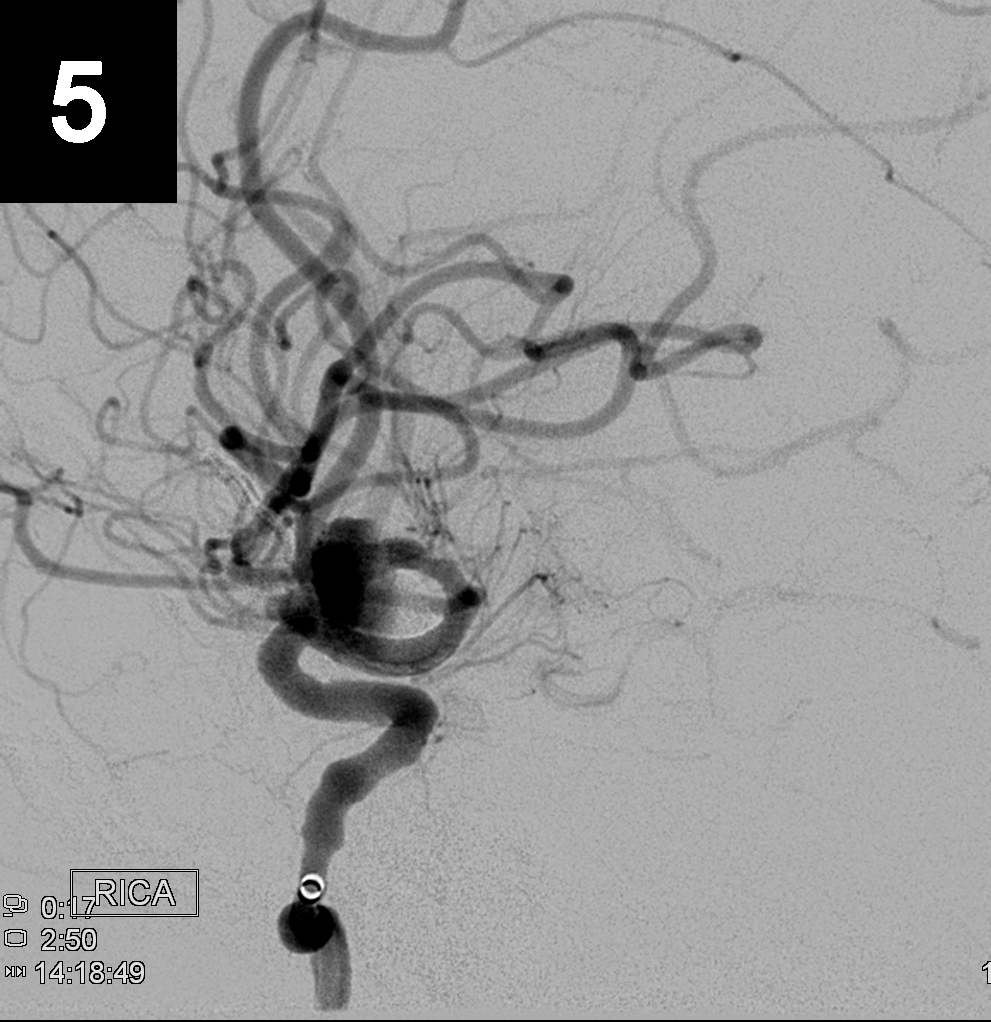
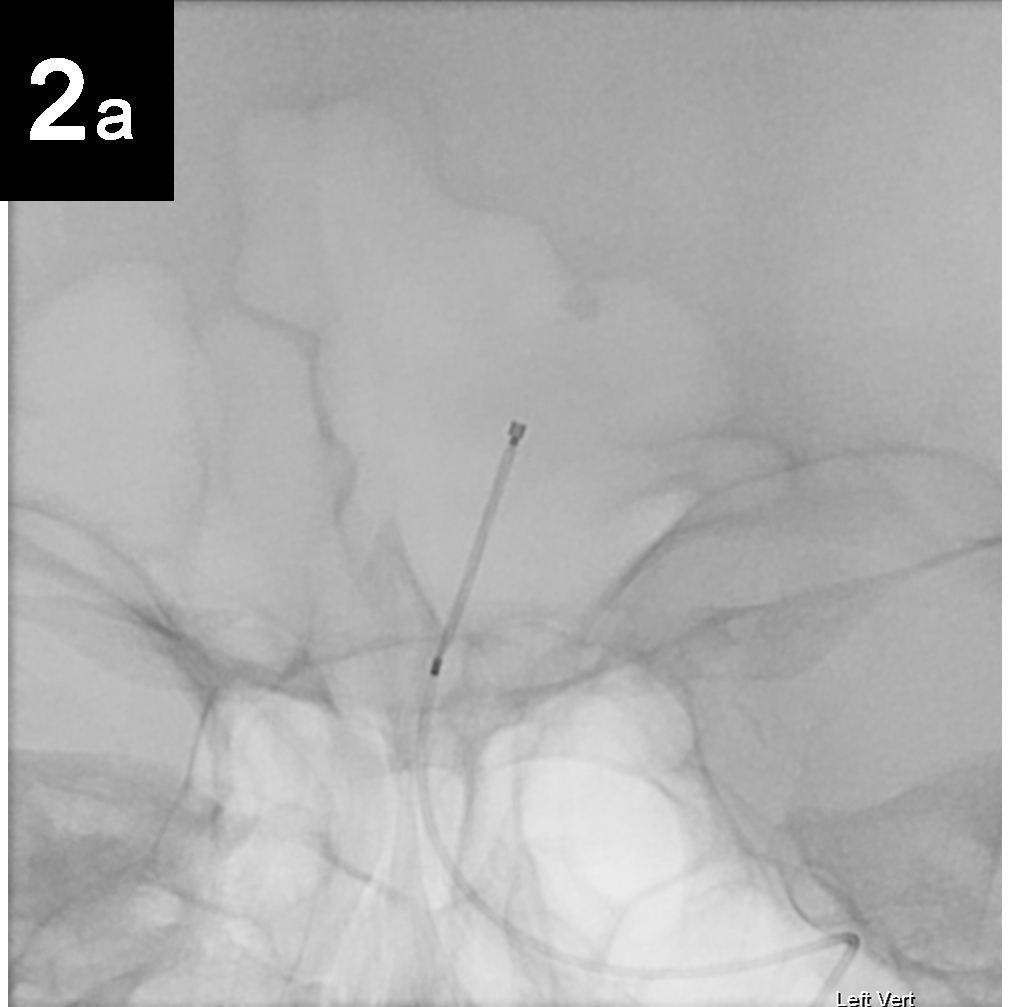
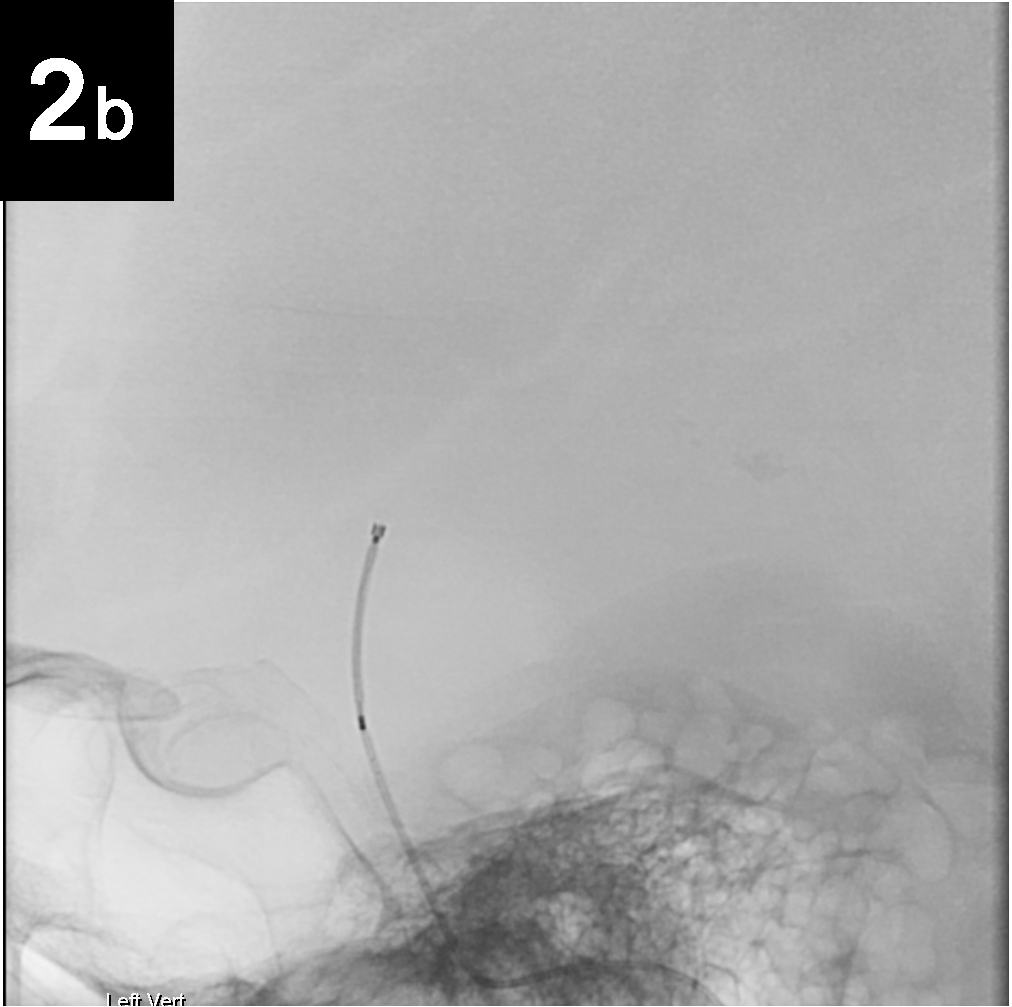
Endovascular Repair
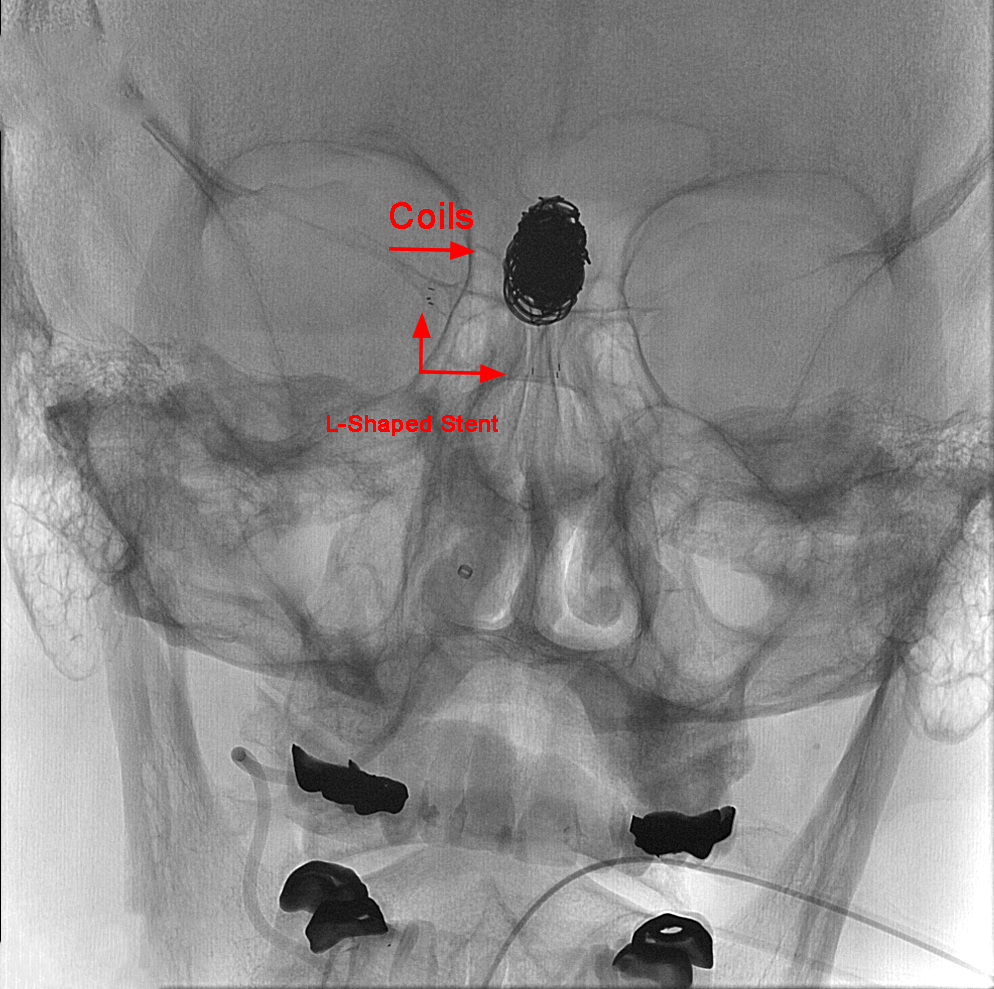
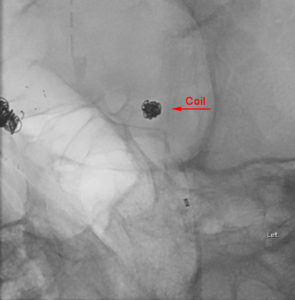
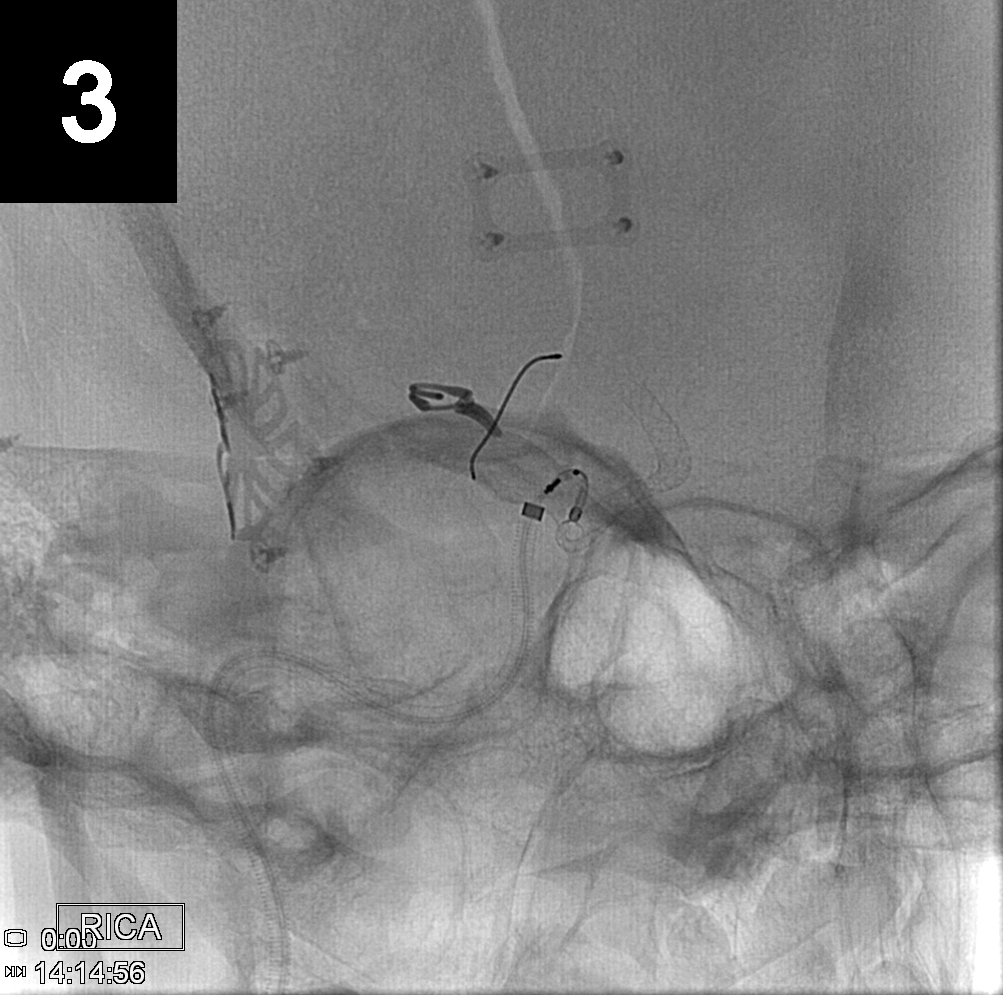
Endovascular (from within the blood vessel) surgery, is performed through a catheter (a hollow, flexible tube) delivered from the groin or leg to the blood vessels in the brain. Thin platinum wires are pushed into the aneurysm, where they conform to the wall of the aneurysm forming a coil mass. Since blood clots form around the coils, the chances of a rupture are greatly reduced. Recovery time is typically only one to three days.
- Primary Coil Embolization:
Treats aneurysm from the inside rather than the outside. Fill aneurysm with embolic coils in order to obliterate blood flow.
Technique
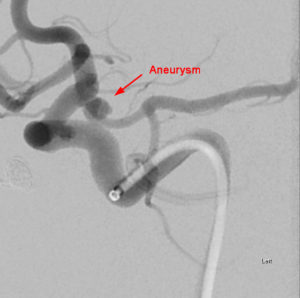
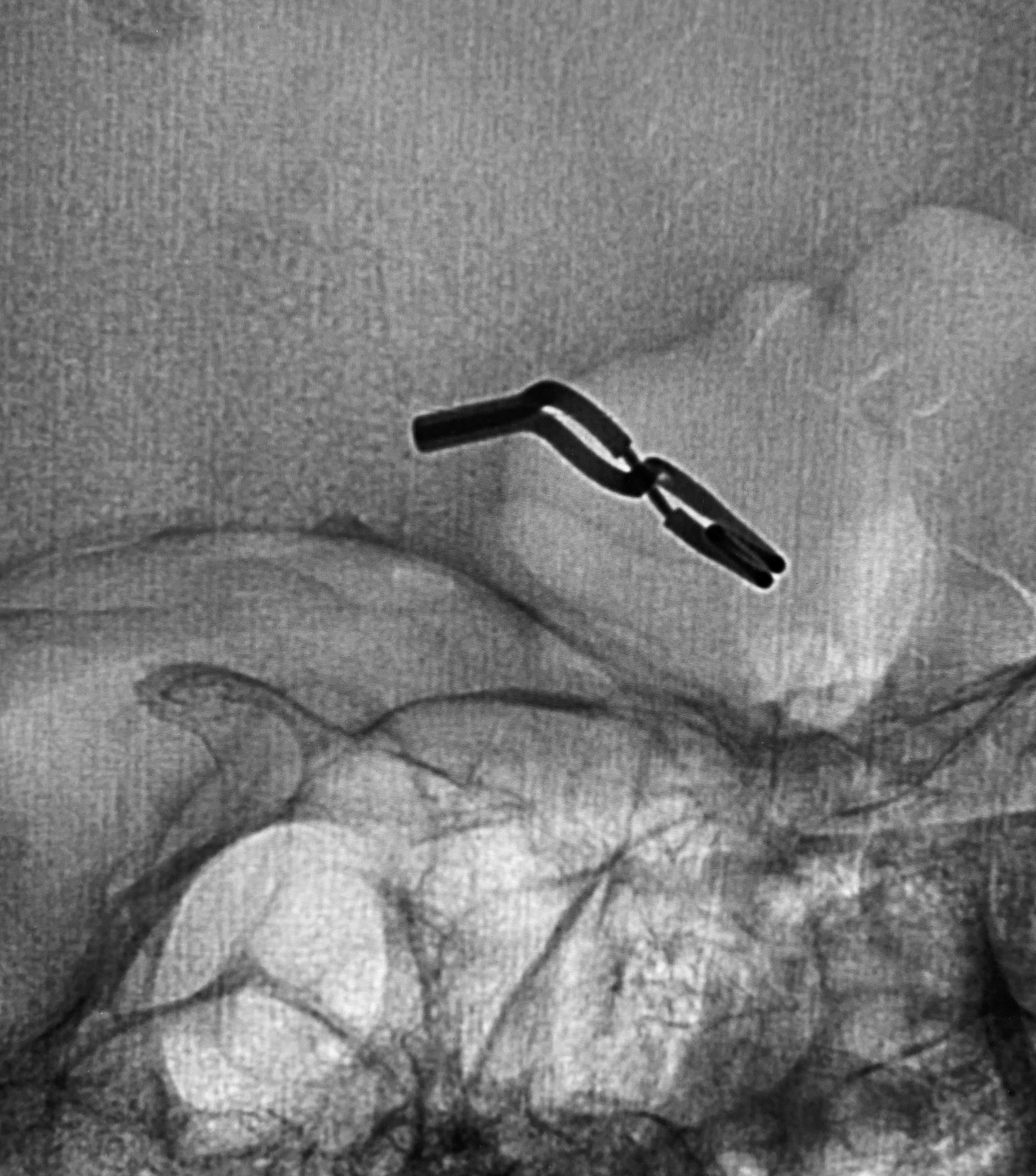
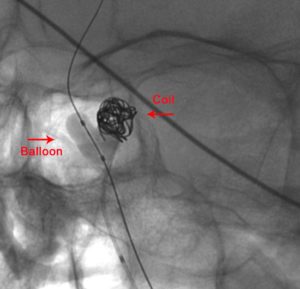
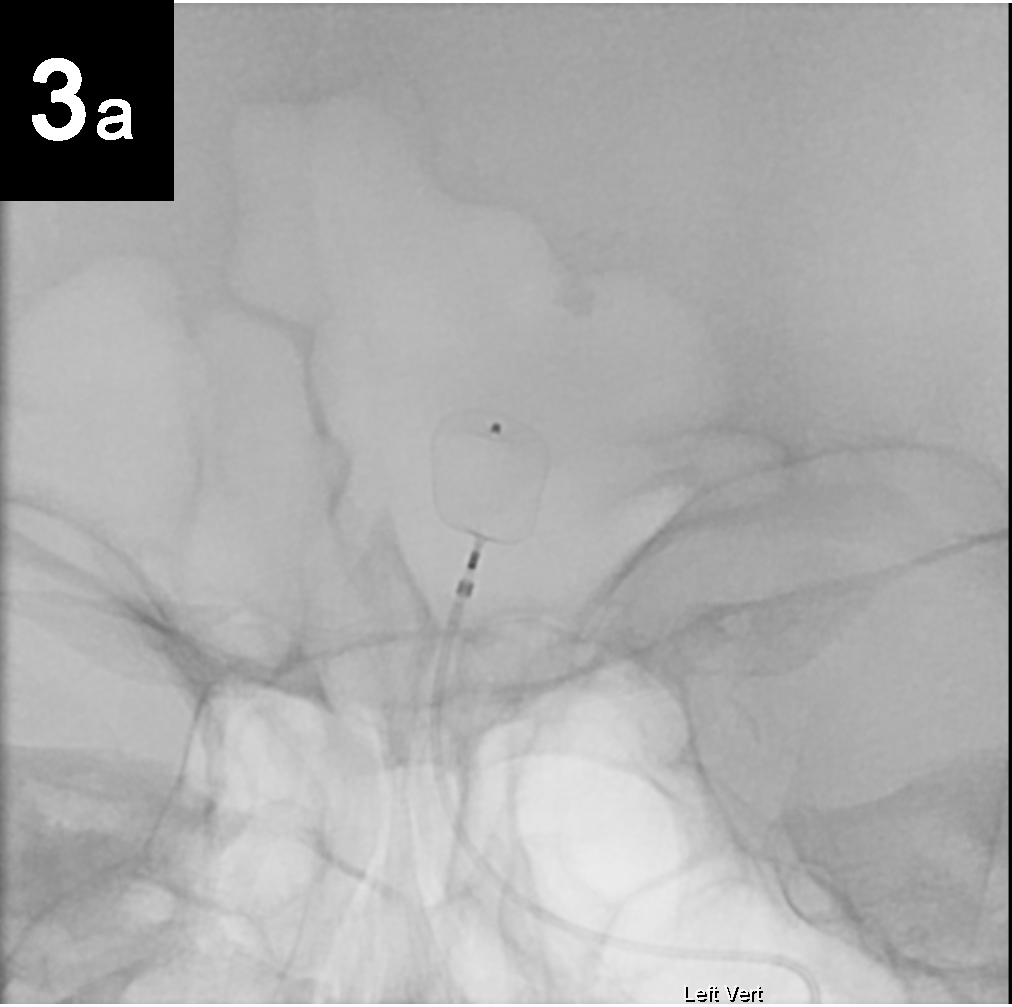
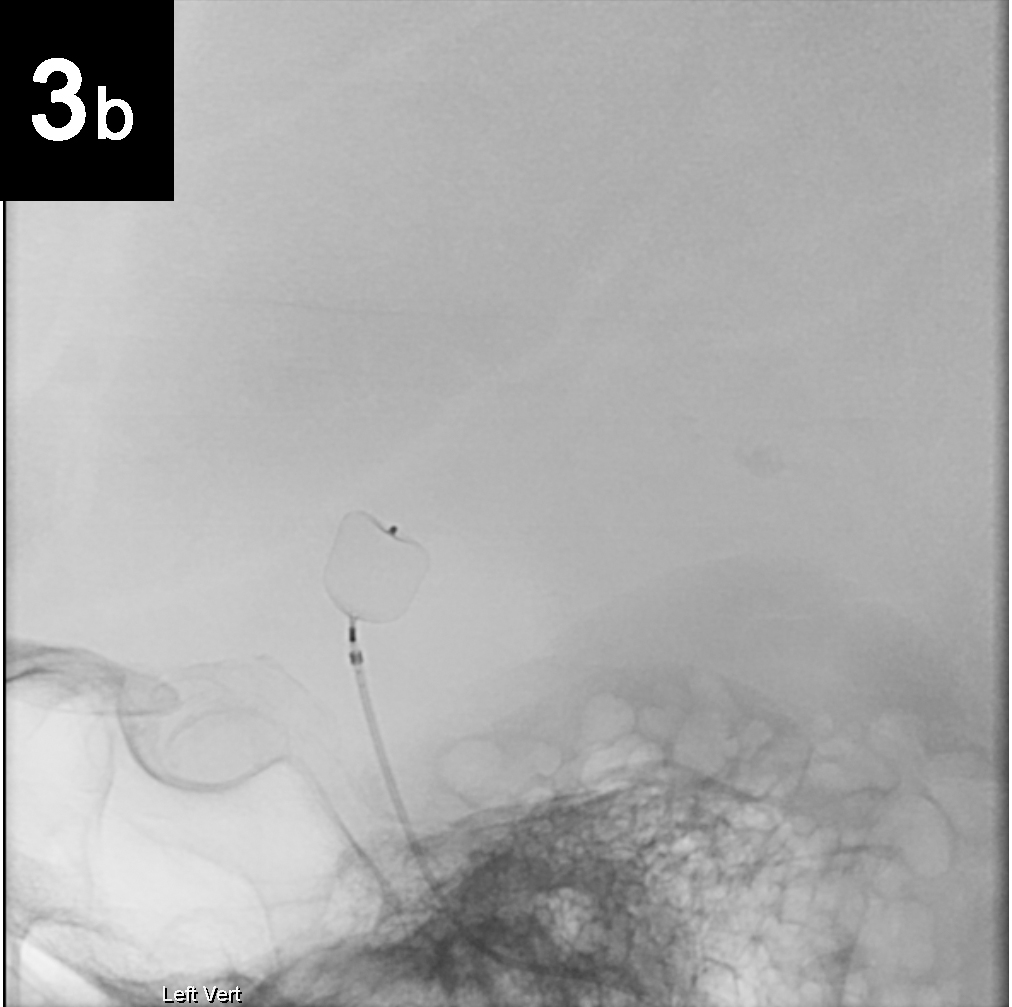
- Balloon Assisted Coiling:
Balloon assisted coiling is used to treat wide-necked (opening too large to keep the coild in place), complex-shaped cerebral aneurysms.

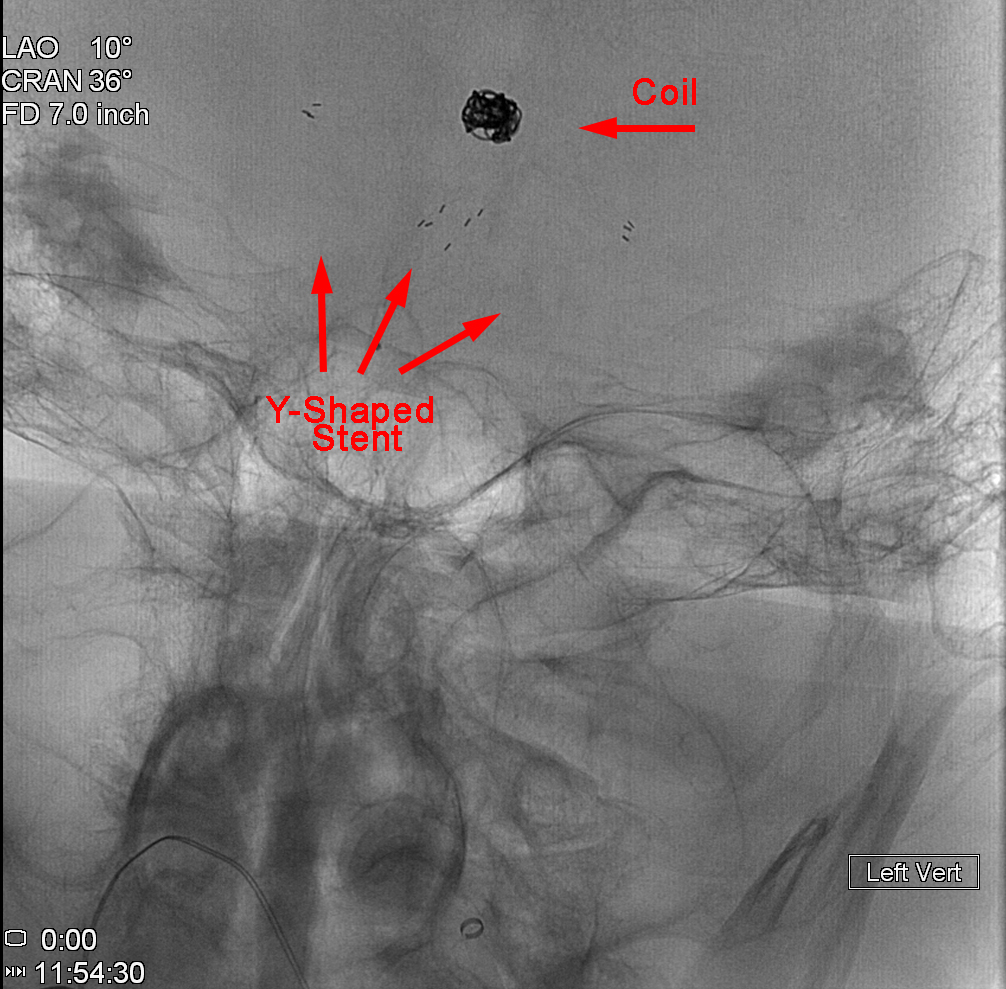
- Stent Assisted Coiling:
Neurovascular stents are intended to treat wide-neck, intracranial, saccular aneurysms.
- Flow Diversion:
Flow diversion is a newer paradigm that involves treating the wall of the parent artery with a special type of stent. This stent diverts flow away from the aneurysm and allows a scaffold for the vessel to repair itself. Flow diversion can be used on unruptured aneurysms only.
Endoluminal:
The Pipeline® Embolization Device allows for true reconstruction of large or giant wide-necked intracranial aneurysms. This device is a fine-mesh stent that diverts blood flow away from the aneurysm causing the blood that remains in the aneurysm to form a blood clot. The clot prevents rupture of the aneurysm and may cause it to shrink over time. Previously, surgical repair of these large and giant aneurysms was difficult, dangerous and sometimes impossible, even for experienced neurosurgeons. The Pipeline Embolization Device provides a potential cure for patients who would otherwise have a very poor long-term prognoses.



Intrasaccular:


LPG Neurosurgery
Rhode Island Hospital
593 Eddy Street
APC Building, 5th Floor
Providence, RI 02903
Phone: (401)-444-8806