Academic Divisions
Overview
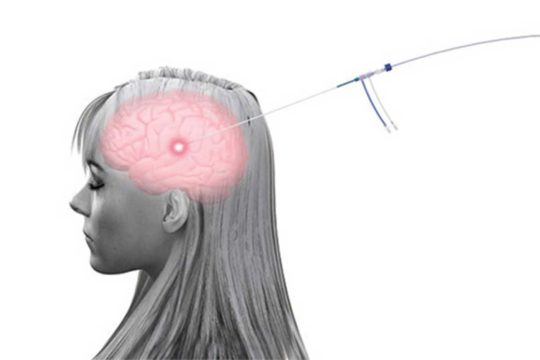
The Division of Functional and Epilepsy Neurosurgery is dedicated to the treatment of neurological and psychiatric disorders through interventions that target and modulate specific brain circuits to improve function and quality of life. Many brain disorders are caused by the dysfunction of specific neural circuits, so applying the latest technologies to modify or repair activity in these circuits can reduce symptoms and restore functions in ways medicine alone often cannot.
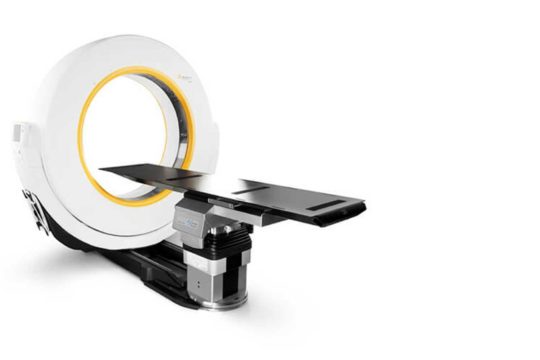
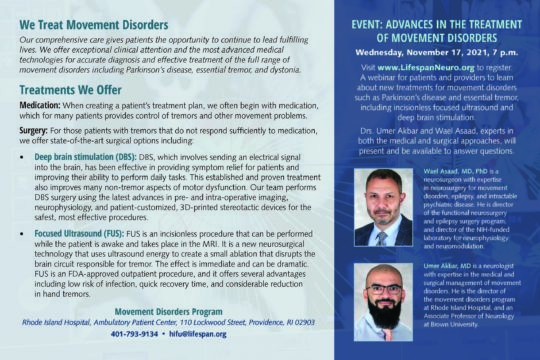
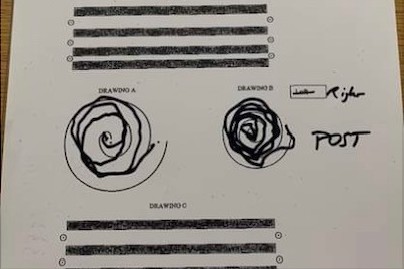
Neurosurgical treatments such as deep brain stimulation, responsive neurostimulation, MRI-guided focused ultrasound and MRI-guided laser ablation are used to treat movement disorders, epilepsy, and intractable psychiatric disease. In addition, novel applications of these technologies to treat cognitive and memory disorders are currently under basic and clinical study within the Brown Neurosurgery program.
Brown University has long been a leader in the basic neuroscience or brain function and in the clinical treatment of functional brain disorders. Ever since Herbert Jasper developed the first EEG laboratory at Brown in the early 1930s, Brown University faculty have continued to pioneer new approaches to study and understand the human brain. These advances include new applications of deep brain stimulation, the first-in-human testing of brain-machine interfaces, and machine-learning innovations to understand neural signals. Brown faculty have elucidated the complex interplay of opposing neural circuits underlying Parkinson’s Disease, the basic mechanisms of frontal lobe function, and the mechanisms of precision motor control. Our division works closely with world-leading faculty in Neuroscience, Neural Engineering, Cognitive Science, and Neuropsychology to better understand basic brain function, to reveal the mechanisms of brain disease, and to develop new, more effective therapies that improve lives.
Major centers and programs within this division include:
Our Team
Director
Neurosurgery Team
Conditions We Treat
Movement Disorders
Psychiatric Disorders
- Intractable OCD
- Intractable Depression (experimental)
- Intractable Tourette’s Disease (experimental)
- Alzheimer’s Disease (experimental)
Clinical Trials
The Functional and Epilepsy Neurosurgery Division undertakes a variety of clinical trials to improve the health of our patients.
Research
Neurosurgery Department
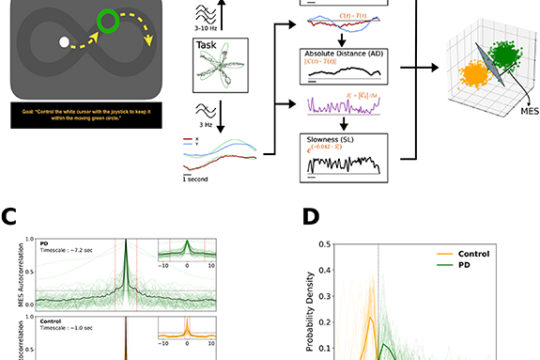
The Computational Neuromodulation Laboratory, Shane Lee, PhD
The Laboratory for Restorative Neuroscience, Athar N. Malik, MD, PhD
Brown Neuroscience and Neuroengineering Collaborators
- David Borton PhD
- John Donoghue PhD
- Michael Frank PhD
- Christopher Moore PhD
- Arto Nurmikko PhD
- Thomas Serre PhD
- Brian Theyel MD, PhD
Technology
Recent News
“Functional neurosurgery aims to restore quality of life to patients with a wide variety of chronic, debilitating neurological disorders.”
– Wael F. Asaad, MD, PhD
Rhode Island Hospital
593 Eddy Street, APC 6
Providence, RI 02903
401-793-9128
401-444-2661