Overview / Multidisciplinary Approach
An arteriovenous malformation (AVM) is a vascular malformation of the brain and spinal cord. Within the vascular system there is a fast (high pressure) delivery of nutrients and oxygen in the arteries and a slow (low pressure) return of waste back to the heart and lungs. Capillaries, nutrient exchange centers throughout your body, are what safely bridge the high pressure arteries to the low pressure veins. In patients with AVM these capillaries are entirely absent and instead there is a dangerous, abnormal connection between the high pressure arteries and the low pressure thinly-walled veins, which are not biologically designed to handle high arterial pressures.
Symptoms
AVM’s are potentially devastating lesions. They are often discovered incidentally through a diagnostic test ordered for another reason, though many people may present with symptoms. Approximately half of all AVM’s come to clinical attention because of a hemorrhage (bleed) into the brain. The remainder present with:
- seizures,
- headaches
- neurological problems such as paralysis, loss of speech, memory or vision
AVM’s that bleed can lead to serious neurological problems and sometimes death. However, some people with these lesions never experience symptoms or complications.
Causes
It is not clear why AVM’s form, but some researchers believe that these tangles of vessels are present from birth (a congenital disorder). Several rare genetic diseases are associated with AVM’s. AVM’s classically appear as a complex tangle of abnormal thinly-walled vessels called a “nidus”. A distinguishing feature is that they occur anywhere within the brain or spinal cord. AVM’s are rare, occurring in about 0.2% of the population (200 cases per 100,000 people).
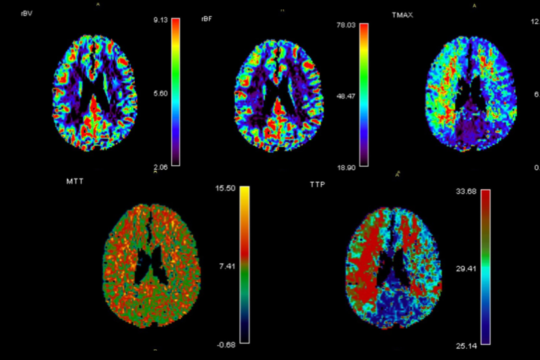
Diagnosis
While a CT (computed tomography) or MRI (magnetic resonance imaging) test of either the brain or spinal cord will typically first detect these lesions, catheter-based diagnostic (cerebral or spinal) angiography is essential to fully understand and characterize the AVM. This evaluation allows your doctor to determine your future risk of symptoms and your treatment options. Treatment of an AVM depends on whether symptoms are present or not, how large the lesion is, where it is located and a host of other features only determined by the diagnostic (cerebral or spinal) angiogram.
Comprehensive Care Center
Treatment Options
- Surgical Resection
Surgical resection can be good choice for some lesions. During a surgical resection, with the help of a high-powered microscope, your neurosurgeon performs a craniotomy (removes part of your skull temporarily), to gain access to the AVM and carefully remove it from the tissues around the brain or spinal cord.
Resection is usually done when the AVM can be removed with little risk of hemorrhage or seizures or cannot be closed with endovascular embolization.
- Radiosurgery
Radiosurgery can be used for smaller, surgically inaccessible lesions.
- Embolization
Historically an adjunctive treatment, Embolization can now be a primary therapy for select lesions. During embolization we pass a catheter through the groin up into the arteries in the brain that lead to the AVM, and inject a material into these arteries that blocks off the artery and reduces the blood flow through the AVM.
Embolization by itself typically does not typically eliminate the AVM and is almost always used as preparation for either surgical resection or stereotactic radiotherapy.
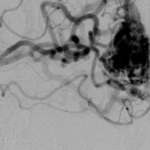
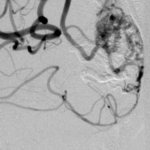
Initial AVM
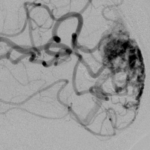
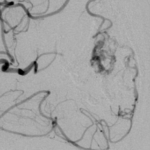
Post-Embolization 1, prior to Gamma Knife Radiotherapy
Post-Embolization 2, prior to Gamma Knife Radiotherapy
Post-Embolization 3, prior to Gamma Knife Radiotherapy
Pre-Embolization prior to surgical resection
Post-Embolization prior to surgical resection
LPG Neurosurgery
Rhode Island Hospital
593 Eddy Street
APC Building
Providence, RI 02903
Phone: (401)-444-8806