Cerebrovascular / Skull Base Surgery /
Academic Divisions
Overview
The Cerebrovascular / Skull Base Surgery / Endovascular Neurosurgery Division encompasses the Departments of Neurosurgery, Interventional Neuroradiology, Neurology, and Radiation Oncology, all of which work together with a focus on a multidisciplinary approach to the treatment and care of various neurovascular diseases (diseases affecting the blood vessels of the nervous system).
We treat conditions that affect blood vessels of the brain, neck, and spine including intracranial aneurysms, extra- and intra-cranial atherosclerostic disease, intracerebral hematoma, arteriovenous malformations (AVM), dural arterio-venous fistulae (dAVF), stroke, moyamoya disease, microvascular compression syndromes such as trigeminal neuralgia, and a host of less common conditions. Our team works to develop individualized treatment plans for each patient, as exemplified by weekly cerebrovascular conference, where patients are discussed and reviewed in detail by the multidisciplinary team. In addition, we have multidisciplinary cerebrovascular clinics every week where our team evaluates all patients in a comprehensive manner. Treatment options range from surgical interventions to more conservative treatment with minimally invasive endovascular procedures such as stenting, radiation therapy, and sometimes prescription medication.
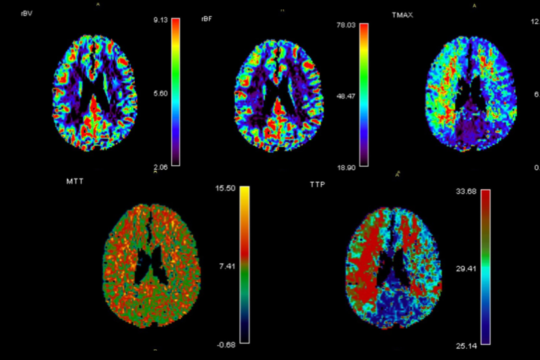
When encountered with a neurovascular condition our team of experts meets and decides on the best treatment available. We have the most advanced imaging capabilities including MRI, non-invasive vascular evaluation with MRA and CTA, detailed evaluation of cerebral blood flow using MR perfusion, and conventional cerebral Angiography. If surgery is required our suites and operative rooms are equipped with advanced intraoperative equipment such as intraoperative CT scanners and surgical microscopes with non-invasive ICG monitoring.
Treatment may include neurointerventional surgery, which means treating the blood vessel disease from within the blood vessel itself, using a catheter and imaging technology to precisely target the condition. Many strokes are treated by removing the blood clot from within the blood vessel in this way. Our division’s clinical research is also deeply involved with outcomes and improving care of these patients, as well as those with complex aneurysms treated using flow diverting device, which is an advanced technique used to treat previously untreatable aneurysms.
Our Team
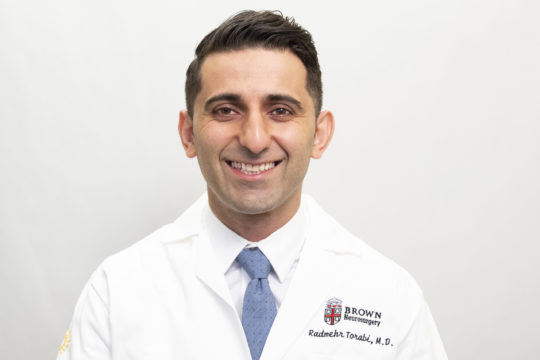
Division Director
Multidisciplinary Team
Combined Neurosurgery and Neuro-Interventional Clinical Faculty
Neuro-Interventional Clinical Faculty
Dylan Wolman, MD
Neurocritical Care
Torrey Birch, MD – Director
Eugenie Attallah, MD
Christoph Stretz, MD
Thanujaa Subramanian, MD
Leslie Kimpler, MD
Radiation Oncologist – Neurosurgical Oncology
Vascular Neurologists
Karen Furie, MD – Chair, Neurologist-in-Chief
Shadi Yaghi, MD
Tina Burton, MD
Elizabeth Perelstein, MD
Christoph Stretz, MD
Farhan Khan, MD
Conditions We Treat
- Ischemic and Hemorrhagic Stroke
- Carotid Disease
- Cerebral and Spinal Aneurysms
- Cerebral and Spinal AVM
- Subdural Hematoma
- Idiopathic Intracranial Hypertension
- Hydrocephalus
- Moyamoya disease
- Cavernous Malformation
- Dural arteriovenous fistulas
- Cerebrospinal fluid venous fistula
Research
- Focus on clinical outcomes and care delivery for patients with ischemic and hemorrhagic stroke, including outcomes after carotid surgery.
- Aneurysm treatment, and in patients treated with thrombectomy for large vessel occlusion.
Technology
- MRI/MR Angiography
- MRI RAPID /MR Perfusion
- CT Angiography
- CT Perfusion
- Cerebral Angiography
- PET scanner
- Intraoperative CT scanner
- Endovascular Aneurysm Treatment
- Coil embolization
- Balloon and stent remodeling
- Flow Diverting Stents
- Intrasaccular flow disruptors
- BrainPath/Myriad Minimally Invasive Clot
Evacuation System - LINAC (radiation therapy)
- Gamma Knife
- CyberKnife
- Surgical microscope with ICG
- AI powered image viewer identifying large
vessel occlusions - Cerevasc Eshunt
- MMA Embolization
- TCAR
- Minimally Invasive Clot Evacuation System
- LITT
- Cerebrospinal fluid venous fistula embolization
- Venous stenting
Rhode Island Hospital
593 Eddy Street, APC 6
Providence, RI 02903
Phone: (401) 793-9166
Fax: (401) 444-2788