About Us
In most respects, the history of neurosurgery in Rhode Island followed the general pattern of the evolution of these specialties throughout the United States. Some limited “brain surgery” was done at first by general surgeons, then formally trained neurosurgeons came to the area. In addition to increasingly sophisticated neurosurgical cases, the early neurosurgeons also handled large amounts of what would now be considered medical neurology, until fully trained neurologists eventually arrived to take over their part of the work. But in Rhode Island, such things often have an interesting and unexpected twist — an individualistic difference — and so it was at the beginning of our story.
In the fall of 1937, Dr. Wilder Penfield, came to Brown to give a talk. He had just recently founded the Montreal Neurological Institute at McGill University, and was already launching into his work in epilepsy surgery that made him famous. On the morning after Penfield’s talk, a young man named Herbert Jasper, PhD, invited Penfield into his laboratory. Jasper, not at that time a physician, had acquired a doctorate in neurophysiology in Paris, where he had seen an early and crude EEG (electroencephalography) machine demonstrate human brain waves through scalp recordings. Jasper was skeptical, and so had constructed his own EEG machine in a basement room at Butler Hospital.
The room was a maze of chicken wire, which served as electrical shielding, and Penfield recalled that, “Inside the maze was a young man [Jasper] moving about like a bird in an aviary.” Jasper told Penfield that he had been able to use the EEG to localize the discharging foci in two epileptic patients. It was then Penfield’s turn to be skeptical, but Jasper was persuasive. A few months later, Penfield operated on Jasper’s Rhode Island patients in Montreal. Jasper’s predictions proved accurate in both cases, and so began one of the most productive and important collaborations in twentieth-century neuroscience.
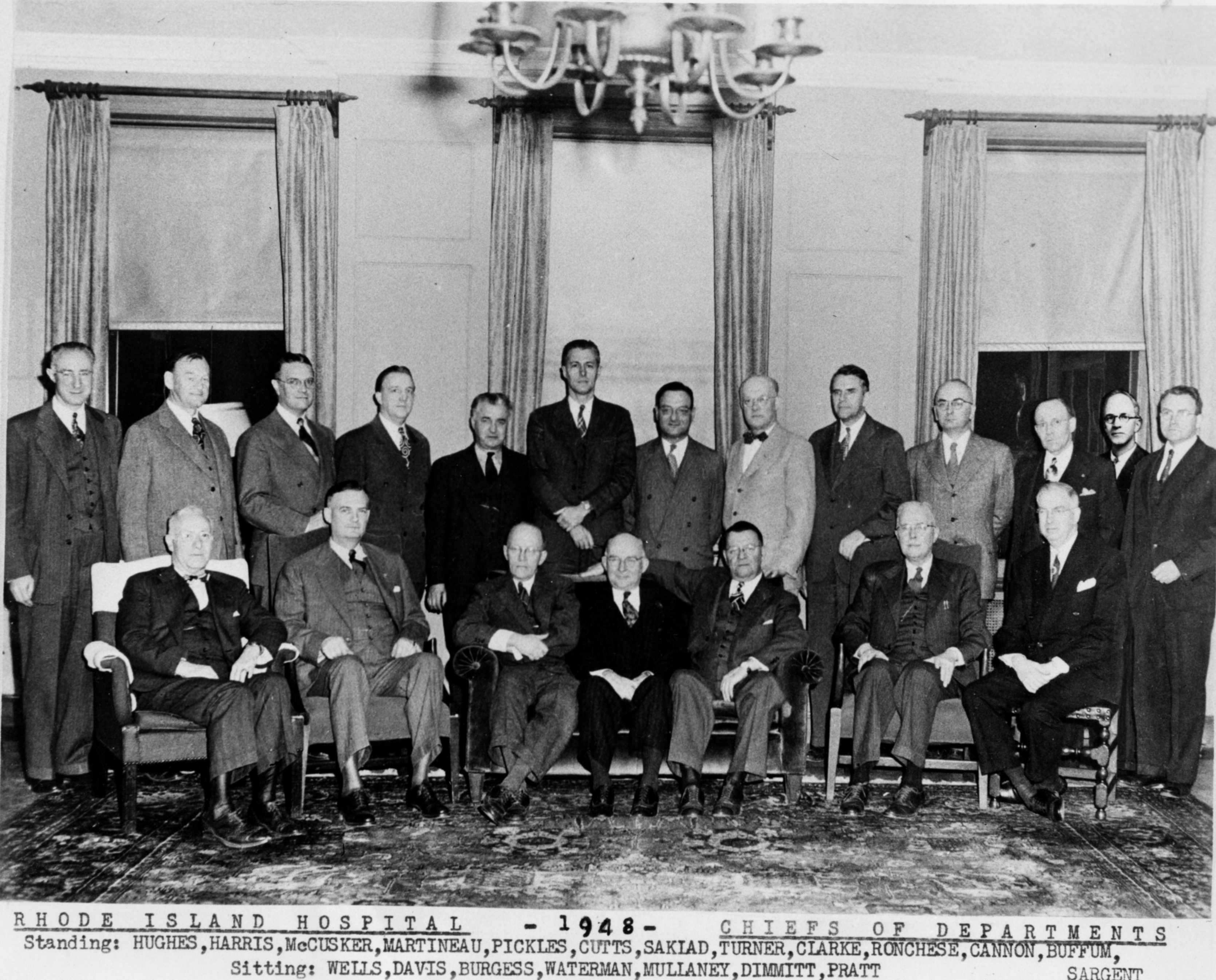
In Rhode Island and at Rhode Island Hospital, the first person to do neurosurgery on a regular basis was Dr. Wilfred Pickles, who had trained as a general surgeon. Dr. Pickles was officially appointed Chief of Neurosurgery at Rhode Island Hospital in 1944. Much of his clinical practice was trauma, and he wrote an important paper on “Acute focal edema of the brain” in the New England Journal of Medicine. The first fully-qualified neurosurgeon in Rhode Island was Dr. Hannibal Hamlin. Hamlin had spent time during his training in Dr. John Fulton’s neurophysiology laboratory at Yale, which was a common part of many neurosurgeons’ experience in those days. When he joined the staff of Rhode Island Hospital in 1947, following Navy service in World War II, Dr. Hamlin obtained a grant to fund clinical research on electrodes in temporal lobe epilepsy.
Dr. Julius (“Gus”) Stoll, Jr. came to Rhode Island Hospital as Hamlin’s associate in 1954. He was not the only force, but a large one, who pushed the idea of having academic neurosurgery and neurology at Brown. He was an important influence behind the development of these programs and he is who we best remember now.
Upon Pickles’ retirement in December, 1956, Stoll became Surgeon-in-Chief of the Department of Neurological Surgery in January, 1957. Stoll received part of his training in Montreal, where he worked with Jasper; they co-authored several papers on epilepsy and neurophysiology. He had turned down an opportunity to join Maitland Baldwin’s surgical epilepsy research program at the National Institutes of Health because he did not wish to limit his practice to temporal lobectomies. He thought he could do both community practice and research, but it proved to be impossible.
In addition to doing neurosurgery and neurology at his home base, he found himself doing many consultations in Attleboro and especially in Fall River, Massachusetts. Eventually he became the senior member of a busy three-man group, including Paul Welch and Melvin Gelch.
Another early arrival on the neurosurgical scene in Rhode Island was Dr. Maurice Silver, who had a background in epilepsy research. Silver was Chief of Neurosurgery at The Miriam Hospital from 1952 to 1960. He was eventually succeeded at that post in 1971 by Dr. Bertram Selverstone, who had trained at Montreal.
 Selverstone developed an outstanding reputation in neurosurgery due in part to his invention of the Selverstone clamp that was used to gradually occlude the carotid artery in the treatment of intracranial aneurysms. In his previous position as Chief of Neurosurgery at the Tufts/New England Medical Center in Boston, Dr. Selverstone had sent a rotating neurosurgery resident to Rhode Island Hospital. This practice was discontinued when the Residency Review Committee decided that the hospitals were geographically too far apart to sustain a viable affiliation. Selverstone had also intended to start a residency program at Brown and The Miriam Hospital, though this initial effort was unsuccessful.
Selverstone developed an outstanding reputation in neurosurgery due in part to his invention of the Selverstone clamp that was used to gradually occlude the carotid artery in the treatment of intracranial aneurysms. In his previous position as Chief of Neurosurgery at the Tufts/New England Medical Center in Boston, Dr. Selverstone had sent a rotating neurosurgery resident to Rhode Island Hospital. This practice was discontinued when the Residency Review Committee decided that the hospitals were geographically too far apart to sustain a viable affiliation. Selverstone had also intended to start a residency program at Brown and The Miriam Hospital, though this initial effort was unsuccessful.
Brown’s six-year program in medicine was initiated in 1963, 133 years after the school’s original medical course had been abolished in 1827. In 1973, the full MD program was re-instituted. The clinical departments were hospital-based and evolved slowly.
Originally, Neurosurgery was a division in the Department of Surgery at both Brown and Rhode Island Hospital. In large part through the efforts of Dr. Stoll, a formal program in Neurosurgery was established in 1985. Dr. Mel H. Epstein came from Johns Hopkins in that year to be its first Chairman.
One of Dr. Epstein’s major contributions was that he understood the Gamma Knife at a time when most people did not. With this understanding, he saw an opportunity to bring the first Gamma Knife to New England. Getting approval for the Gamma Knife required pushing through the hospital administration and the state bureaucratic apparatus. There were obstacles along the way, and Epstein met each resistance head on. Eventually, Rhode Island Hospital obtained one of the first Gamma Knives in the country. The first director of the Gamma Knife, Christer Lindquist, had been trained by its brilliant inventor, Lars Leksell.
The Gamma Knife became a signature of the program, something special that the hospital and the program had to offer. The only similar treatment nearby was the proton beam apparatus at Massachusetts General Hospital, which could not perform highly focused treatments such as stereotactic radiosurgery.
The Neurosurgery Research Laboratory was also established in 1985 with the recruitment of Conrad Johanson, PhD, a senior investigator with extensive experience in cerebrospinal fluid (CSF) research.
In 1987, the Neurosurgery Residency Program was approved; it was a seven-year residency. Six slots in that first year were filled with residents who transferred from other programs. The very first resident to go through all seven years was Dr. Deborah Benzil, one of the founders of WINS (Women in Neurosurgery) and now a prominent, nationally recognized neurosurgeon. She began the program in 1987 and graduated in 1994. The residents were accomplished, with the likes of Dr. Michael Park winning the Van Wagenen Traveling Fellowship Award from the American Association of Neurosurgeons (AANS).
Board-approved residencies in neurosurgery and neurology were instituted, and the programs in neurosurgery and neurology were combined into the Department of Clinical Neurosciences with Drs. Easton and Epstein, who alternated administrative responsibilities every two years as Co-Chairmen.
 In 1988, the Julius Stoll Chair of Neurosurgery was endowed to support the Neurosurgeon-in-Chief at Rhode Island Hospital. This was funded in part by a generous contribution from its namesake and in part by the many friends of Dr. Stoll, who wished to recognize his tireless efforts on behalf of the clinical neurosciences at Brown and throughout the Rhode Island medical community.
In 1988, the Julius Stoll Chair of Neurosurgery was endowed to support the Neurosurgeon-in-Chief at Rhode Island Hospital. This was funded in part by a generous contribution from its namesake and in part by the many friends of Dr. Stoll, who wished to recognize his tireless efforts on behalf of the clinical neurosciences at Brown and throughout the Rhode Island medical community.
After Dr. Epstein retired in 2001, Dr. John Duncan, a pediatric neurosurgeon, became the Chair of the Department of Neurosurgery.In 2010, Dr. Rees Cosgrove, a functional neurosurgeon, was appointed as Chair of the Department. He reorganized the Department, recruited two new faculty, Drs. Wael F. Asaad and Albert E. Telfeian, and was instrumental for the establishment of the Norman Prince Neurosciences Institute. In 2015, Dr. Ziya Gokaslan, world renowned for building the spine program at Johns Hopkins, was named Chairman of the Department of Neurosurgery. Since that time, there has been a tremendous increase in faculty and technology, over 220 departmental publications, an increased focus on multi-subspecialization, and the development of a fellowship program, to name a few accomplishments.
Neurosurgery in Rhode Island, especially in the Department of Neurosurgery at Rhode Island Hospital and our affiliate locations, from its beginning to its technologically advanced present, strives to provide some of the best patient care and neurological innovation in the country and in the world.
Former Chairmen:
Mel H. Epstein, MD
John Duncan, MD
Rees Cosgrove, MD
Professor Emeriti:
Samuel Greenblatt, MD
